These webpages aim to provide practical information to help people who are at the end of their lives, and those supporting them, to access the right information at the right time.
Information is for use across South Yorkshire, including Barnsley, Doncaster, Rotherham and Sheffield. Where information is specific to a particular city or town, we will clearly indicate this.
These pages contain:
-
materials you may want to use for planning ahead and information on ReSPECT
-
support available, including specialist services
-
details on where to seek support and advice
-
Bereavement & grief information
Information contained in these webpages is a response to what members of the public and professionals told us they needed.
What is palliative care?
Palliative care is defined by the World Health Organisation as an approach that improves the quality of life of patients (adults and children) and their families who are facing problems associated with life threatening illnesses.
It prevents and relieves suffering through the correct assessment and treatment of pain and other problems, whether physical;, psychological, or spiritual.
You may find these videos provide an introduction and helpful information:
Palliative care improves the quality of life of patients with life-threatening illness
A more detailed explanation What you need to know about Palliative Care

What is end of life care?
NHS explains that end of life care is support for people who are in the last months or years of their life.
End of life care should help you to live as well as possible until you die and to die with dignity. The people providing your care should ask you about your wishes and preferences, including where you may want to receive your care and take these into account as they work with you to plan your care.
They should also support your family, carers or other people who are important to you.
Palliative and end of life care can help with many things including -
-
early identification of your illness and understanding its progression (is it getting worse?)
-
offering support with decision making and advance care planning,
-
addressing physical symptoms such as pain management, movement and eating and drinking
-
psychosocial and spiritual support,
-
bereavement & grief support.
Support to those who need palliative and end of life care is available across the whole of South Yorkshire, with many medical, social care, community, and voluntary organisations available to help and support everyone, whatever age, gender, ethnicity, religion, or wherever you live.
Palliative and end of life care is provided in a number of different locations, including in the home, in care and nursing homes, in each hospital across South Yorkshire, some specialist clinics and in hospices.
There are often a lot of people involved. Many we have spoken to often have 10 to 15 different people and / or organisations involved in their care. Sometimes you may hear a phrase called a multi-disciplinary team, which may include doctors, physiotherapists, occupational therapists, social workers, nurses, district nurses, speech therapists, dietitians and psychologists.
Other organisations you may also come into contact with may include
-
organisations who provide medical and practical equipment,
-
the ambulance service and paramedics if there’s an emergency,
-
your local pharmacy
-
those who come into your home and care for your where you live.
Support by those closest to you
For those at the end of life and those caring for them, many people find the support offered and provided by family, friends, neighbours, colleagues, peers, spiritual leaders and community groups invaluable.
The people providing your care should ask you about your wishes and preferences and take these into account as they work with you to plan your care.
They should also support your family, carers or other people who are important to you.
Information is taken from NHS Changes in the last hours and days - NHS
Changes in the last hours and days of life
Dying for Beginners | Dr Kathryn Mannix
Physical changes are likely to happen when you're dying. These happen to most people during the terminal (dying) phase, whatever condition or illness they have. This can last hours or days.
Becoming drowsy
You'll start to feel more tired and drowsy and have less energy. You'll probably spend more time sleeping, and as time goes on you'll slip in and out of consciousness.
Not wanting to eat or drink
Not wanting to eat is common in people who are dying. You may also find it difficult to swallow medicine.
Your healthcare professionals can discuss alternative ways of taking medicine with you and your carers, if necessary.
Your family and carers may find it upsetting or worrying if you do not eat, especially if they see you losing weight, but they do not need to make you eat.
As you get closer to dying, your body will not be able to digest food properly and you will not need to eat.
If you cannot swallow your drink, your carers can wet your lips with water.
Changes in breathing
Your breathing may become less regular. You may develop Cheyne-Stokes breathing, when periods of shallow breathing alternate with periods of deeper, rapid breathing.
The deep, rapid breathing may be followed by a pause before breathing begins again.
Your breathing may also become noisier as a result of the build-up of mucus.
The body naturally produces mucus in your breathing system, including the lungs and nasal passages. When you're healthy, this mucus is removed through coughing.
When you're dying and no longer moving around, the mucus can build up and cause a rattling sound when you breathe.
Confusion and hallucinations
Medicines or changes in the chemical balance of your brain can cause confusion or hallucinations.
A hallucination is when you see or hear things that are not there. If you become confused, you may not recognise where you are or the people you're with.
Some people may be restless or seem to be in distress. For example, they may want to move about, even though they are not able to get out of bed, or they may shout or lash out.
This can be out of character and distressing for family and carers.
The medical team can rule out or treat any underlying causes, such as pain, breathing problems or infection, or calm the person who is dying.
If no underlying cause can be identified, there are medicines that can ease distress.
Cold hands and feet
The feet and hands may feel cold because of changes in your circulation. Blankets over the hands and feet can keep you warm.
People with lighter skin tones may look slightly blue. On people with darker skin tones, it may be easier to see any blue tone on their lips, nose, cheeks, ears, tongue or inside their mouth.
Practical information (links to helpful information)
Receiving end of life care at home
Your GP can arrange for community nurses to come to your home and provide nursing care for you there. You may also need specialist care from community palliative care nurses who visit you at home to:
-
provide or arrange hands-on nursing or personal care, if you need it
-
advise on pain and symptom control
-
provide practical and emotional support for you and your carers at home
They can also involve other specialist professionals in your care if their expertise is needed.
Your local authority's social services department may provide a range of services and equipment to help you remain at home as you approach the end of life. This could include home adaptations, such as handrails.
Hospice care
The aim of hospice care is to improve the lives of people who have an incurable illness.
Hospices provide care for people from the point at which their illness is diagnosed as terminal to the end of their life, however long that may be.
That does not mean hospice care needs to be continuous. People sometimes like to take a break from hospice care if their condition has become stable and they are feeling well.
Hospice care places a high value on dignity, respect and the wishes of the person who is ill. It aims to look after their medical, emotional, social, practical, psychological, and spiritual needs, and the needs of the person's family and carers. Looking after all these aspects is often referred to as "holistic care".
Care also extends to those who are close to the patient, as well as into the bereavement period after the patient has died.
Where is hospice care provided?
Hospice care is available across South Yorkshire to people of all ages. The local adult hospices are as follows
- Barnsley Hospice,
- St Johns Hospice Doncaster,
- Rotherham hospice
- St Luke’s hospice in Sheffield for adults.
- For children Bluebell Wood is the children’s and young people’s hospice for South Yorkshire.
Hospices have a range of services which are delivered in the following settings -
-
in the home,
-
in care homes,
-
at the hospice itself,
-
as a day patient visiting the hospice.
-
other environments e.g. hostels.
Hospice care is a style of care. Hospice teams might include doctors, nurses, healthcare assistants, social workers, therapists, counsellors, chaplains and trained volunteers.
Hospices aim to feel more like a home than hospitals do. They can provide individual care more suited to the person who is approaching the end of life, in a gentler and calmer atmosphere than a hospital.
What does hospice care cover?
The services that hospices offer vary, but most offer medical and nursing care, including managing pain and other symptoms. They might also offer:
-
complementary therapies, such as massage
-
rehabilitation – helping you remain independent through things like physiotherapy
-
respite care– looking after you so your carers can have a break from caring for a short while
-
information about coping financially
-
bereavement care
-
spiritual and psychological help
The staff at most hospices will be happy to talk to you about what the hospice offers or show you around the facilities if you are considering hospice care. The staff can discuss any issues with you and answer questions.
When does hospice care start?
Some people think that you only have hospice care when you are dying, but this is not true.
A hospice palliative care team might help control symptoms such as pain or breathlessness early on in your illness, with you staying at the hospice for a few days before going home again.
Or you might go into the hospice so that your family or carers can have a break from looking after you for a short while. This is called respite care. But not all hospices offer this service. Ask your local hospice if it can offer you respite care. Please see the ‘Support for Adults’ section below for details about your local Hospice.
Some people have a number of periods of hospice care, depending on their condition and their wishes.
Hospice care is free, paid for through a combination of NHS funding and public donation. You can contact a hospice directly yourself, but the team will usually also ask for a referral from your doctor or nurse. Places are limited, but you can contact your local hospice to see what is available.
End of life care in a care home
You can receive palliative and end of life care in a care home. There, trained staff should be available to look after you day and night. They can provide the same type of care you may have been receiving at home, such as help with washing, dressing and providing meals.
Some care homes provide skilled nursing care to residents when they need it. These are sometimes called nursing homes, and they are suitable for people who have a disability, a serious long-term condition or very restricted mobility.
Care homes can be run by:
-
voluntary organisations
-
private individuals
-
private companies
-
the local council
Care homes near you
Palliative care is also offered in care homes in a similar way to that delivered in the home.
How do I find a care home?
Finding a care home can be a challenge, particularly if this is not something you have done before. Care homes all offer a different environment and finding the right one for you / the person you are caring for can be daunting.
You can talk to your local council's adult social care services department, GP or district nurse, palliative care team, or your hospital doctor or nurse to find out what is available in your area.
For care home information in Doncaster Care homes for older people - City of Doncaster Council
For care home information in Sheffield - Residential and nursing care | Sheffield City Council
For care home information in Rotherham Find a care home – Rotherham Metropolitan Borough Council
For care home information in Barnsley Live Well Barnsley | Directory
When looking for a care home, this checklist has a list of questions you may find useful to ask:
-
What does the Care Quality Commission (CQC) say about the service?
-
Do the care home staff receive regular end of life care training?
-
What are the arrangements for care and support from the GP and community nurses, both for routine care and for emergencies?
-
Does the care home participate in a service improvement programme run by local health or social care services?
-
What is their end of life care approach and are they accredited by any standards, for example the Gold Standards Framework?
End of life care in hospital
In hospital, you will be cared for by the doctors, nurses and other healthcare professionals who work on the ward where you are staying.
In South Yorkshire there are specialist palliative care teams in each hospital offering expertise in palliative units and across the hospital. In Sheffield Teaching Hospitals, there is a specific Palliative Care Unit.
Palliative care teams provide hospital staff with specialist advice on pain and symptom control. They can also help staff with your discharge plan, or your transfer to a hospice, community hospital or care home.
When there is no cure for an illness, palliative and end of life care aim to make the end of your life as comfortable as possible. The staff caring for you in hospital should give you high-quality end of life care, tailored to your individual needs.
They should involve you and the people close to you in decisions about your care. They can explain to you what is going on and should make sure they understand and communicate with each other about your choices and preferences.
If there is anything you want to know, ask your doctor or nurse. If they do not know the answers to your questions, ask them to find somebody who does.
Managing pain and other symptoms during end of life care
Managing symptoms, including pain, is an important part of end of life care. Each person will have different symptoms, depending on their condition and the kind of treatment they may be having.
Symptoms can include feeling and being sick, constipation, loss of appetite and pain.
Your doctor and nurses will help you manage your symptoms and feel as comfortable as possible.
Pain
Not everyone approaching the end of life has pain. If you do, your doctor or nurse will assess the pain and decide on a suitable medicine and the correct dose to manage it. They'll ask you questions about the pain.
These might include:
-
where the pain is
-
when it started
-
the effect it's having on you – for example, whether it's stopping you sleeping
If you have trouble speaking, they may use a different method, like a visual chart or picture cards, or ask your family and carers.
If you're not able to communicate at all, there are other signs that can show you might be in pain, such as grimacing, groaning, changes in breathing and refusing to eat.
The doctor or nurse will sometimes ask the palliative care team to advise them.
You can find out more about managing pain and symptoms on the NHS website: Managing pain and other symptoms - NHS
Living and coping with a terminal illness
There's no right or wrong way to feel when you're told you have a terminal illness, which is a health condition that cannot be cured and that you'll most likely die from. You might feel numb at first, and unable to take in the news, or feel calm and matter-of-fact about dying.
Your feelings
As time passes, you may experience a range of emotions. It's normal to feel some or all of the following:
-
shock
-
fear
-
anger
-
resentment
-
denial
-
helplessness
-
sadness
-
frustration
-
relief
-
acceptance
You may also feel isolated and alone, even if you have family and friends around you.
You might not experience all of these feelings and, if you do, they'll not necessarily come in any particular order. Whatever you feel, you do not have to go through it alone.
You can find out more on the NHS website: Coping with a terminal illness - NHS. The Marie Curie website also has helpful information about living with a terminal illness: Living with a terminal illness | Information and support | Marie Curie
Click here for the list of support services available for adults in Barnsley.
Click here for a list of support services available for adults in Doncaster.
Click here for a list of support services available for adults in Rotherham.
Click here for a list of support services available for adults in Sheffield.
My Personal Wishes
Use My Personal Wishes to help you share what matters most to you, your wishes, feelings, beliefs, and values. It’s a helpful way to make sure everyone knows what matters to you and can work together to respect your choices.
You can
- Use it to write down your thoughts about future care and treatment, and it’s okay to take your time.
- Fill it in on your own or with someone you trust and update it whenever things change.
- Share with your family, friends, and the professionals supporting you.
Please keep this document with your ReSPECT plan and other important papers so it’s easy to find when needed.
Tips
1. Start the conversation
Discuss your wishes with your partner, family, carers, and health professionals.
2. Explore your options
Think about:
- What’s important to you in everyday life
- Your thoughts about future care and treatment
- Where you would like to be cared for
- Any questions or worries about illness or dying
- What you want, and what you do not want to happen
- Who you would like to speak for you if you cannot
- Funeral preferences
- Memory-making ideas (e.g., memory boxes, letters, videos)
Additional things to consider:
- Legal and financial matters: Making a will or planning for dependents
- Refusing specific treatments: Using an Advance Decision to Refuse Treatment (ADRT)
- Appointing someone to decide for you: Setting up a Lasting Power of Attorney (LPA)
3. Review and update regularly
Your wishes may change over time—update your plan whenever you need to.
Need any further help?
Go to the content on
- Why plan ahead
- What is advance care planning
What is ReSPECT?
 Click here to learn about what ReSPECT means.
Click here to learn about what ReSPECT means.
You can also watch this video to introduce you to ReSPECT.
ReSPECT stands for Recommended Summary Plan for Emergency Care and Treatment. The ReSPECT process creates a personalised recommendation for your clinical care in emergencies where you are not able to make decisions or express your wishes.
A ReSPECT plan is created through conversations between you and one or more of the health professionals who are involved with your care. The recommendation should reflect both patient preferences and clinical judgement.
ReSPECT is used across a range of health and care settings, including your own home, an ambulance, a care home, a hospice, or a hospital.
The ReSPECT process is adopted across South Yorkshire.
What does a ReSPECT plan look like?
This link will take you to an example of a ReSPECT plan: ReSPECT_v3-1_Form_Specimen_FINAL.pdf
The ReSPECT plan will be completed and then printed off for you and will either be purple or black. Both colours are okay and can be used.
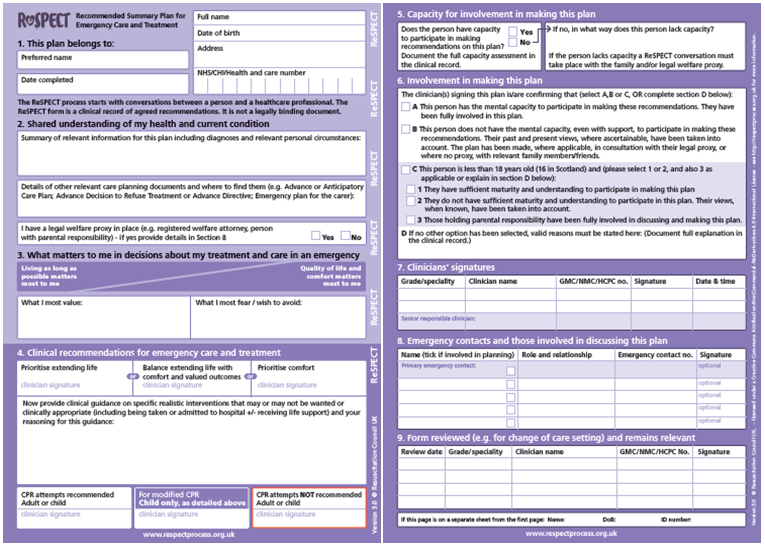
Who is ReSPECT for?
ReSPECT can be for anyone who wants to record their care and treatment preferences but will be particularly relevant for those who have complex health needs, are likely to be nearing the end of life, or at risk of sudden deterioration or cardiac arrest.
How does ReSPECT work?
The ReSPECT process involves you having a conversation with your healthcare professionals. Together you’ll produce recommendations about the types of care and treatment you would or would not want to be considered in an emergency, and which would not work or be of overall benefit to you.
You may also wish to include your family and/or carer(s) in these discussions.
The agreed plan is recorded on a ReSPECT form. If your condition changes, or you change your mind, you can speak to your clinician again, who will update your plan.
Helpful tips
- A printed copy should stay with you and be available immediately to any healthcare professionals called to help you in an emergency, whether you are at home or being cared for elsewhere.
- If you go to hospital, take the ReSPECT plan with you.
- Professionals such as ambulance clinicians, out-of-hours doctors, care home staff, and hospital staff will be better able to make quick decisions about how best to help you in an emergency, if they can refer to your ReSPECT plan.
Further information
For more information about ReSPECT, please see the Resuscitation Council’s website: ReSPECT for patients and carers | Resuscitation Council UK
You can view and download useful easy read documents via the links below:
- Easy Read Guide: Leaflet 1 - Introduction
- Easy Read Guide: Leaflet 2 – Making choices
- Easy Read Guide: Leaflet 3 – Making a ReSPECT Plan
- Easy Read Guide: Leaflet 4 – Two stories – Mark & John
You can view and download useful guides via the links below:
- ReSPECT Patient guide – for adults
- ReSPECT Parent guide – for families of children and young people
- ReSPECT Patient guide – for young people
To learn more about ReSPECT and how it can help you, your family, and friends, please visit the Resuscitation Council UK’s website: ReSPECT for patients and carers | Resuscitation Council UK
(reference www.NHS.uk)
Why plan ahead for end of life care?
Planning ahead can help you receive the care you want and can also help to make things easier for your partner or family when you're nearing the end of life.
Advance care planning is a process. It includes thinking, talking and recording your wishes about what care and support you may want in the future. The plan can be used to help you and those caring for you to inform decision making and in case there's a time when you're unable to take part in the discussions and decision-making yourself.
Many people feel uncomfortable talking about their wishes for the end of their life, however not talking about it denies the person the opportunity to fully participate in discussions and decisions about their current and future care.
Advance care planning can be done at any stage in life. Clare Fuller recommends if you are making an Advance Decision to Refuse Treatment (ADRT) or a Lasting Power of Attorney (LPoA) then it’s a good idea to also write an advance care plan, or a statement of your wishes. You can do this by using a template, purchasing a book, or just writing on a piece of paper by following our tips on how to make an advance care plan, and using our advance care planning templates and tools which can be found further down on this page.
What is advance care planning?
The Gold Standards Framework video provides an overview in 5 Simple Steps https://youtu.be/i2k6U6inIjQ.

The 5 steps are -
- Think
- Talk
- Record
- Discuss
- Share
Compassionate Sheffield has an introduction to advance care planning video which may be helpful. You can view it here. This is also available in a number of languages (Arabic, Urdu, Swahili, Bengali, Slovak Roma). You can find these videos here.
This Advance Care Planning: Getting Your House in Order image may help you to work through your Advance Care Plan.

You can download the image here.
Principles for Advance Care Planning
There are six universal principles for Advance Care Planning NHS England » Universal Principles for Advance Care Planning (ACP)
- The person is central to developing and agreeing their advance care plan including deciding who else should be involved in the process.
- The person has personalised conversations about their future care focused on what matters to them and their needs.
- The person agrees the outcomes of their advance care planning conversation through a shared decision-making process in partnership with relevant professionals.
- The person has a shareable advance care plan which records what matters to them, and their preferences and decisions about future care and treatment.
- The person has the opportunity, and is encouraged, to review and revise their advance care plan.
- Anyone involved in advance care planning is able to speak up if they feel that these universal principles are not being followed.
An easy read version can be found here.
NHS website explains that an advance decision (sometimes known as an advance decision to refuse treatment, an ADRT, or a living will) is a decision a person can make now to refuse a specific type of treatment at some time in the future. It lets the person’s family, carers and health professionals know their wishes about refusing treatment if they’re unable to make or communicate those decisions themselves. The treatments they are deciding to refuse must all be named in the advance decision. A person may want to refuse a treatment in some situations, but not others. If this is the case, they need to be clear about all the circumstances in which they want to refuse this treatment.
An advance decision is not the same as an advance statement. Advance decision (living will) - NHS
Your ADRT should be known to those caring for you and your family, and those close to you. The information below is provided with permission by Clare Fuller, https://speakforme.co.uk/advance-care-planning-explained
Why it matters
An ADRT gives you peace of mind in knowing you will not receive a treatment in the future that you may wish to refuse.
For many people this can give a sense of control and peace of mind
How to do it
You can make an ADRT yourself; to ensure it is legal:
- You must be over 18 and have capacity.
- The Advance Decision to Refuse Treatment must be written down, signed and witnessed
- It must also have the following statement "I confirm the following refusal of treatment even if my life is at risk or may be shortened as a result”
When to consider it
After the age of 18 and at any stage of life.
If you know there is a “hard line” or a treatment that you would not wish to have under any circumstance.
Following diagnosis of a long-term health condition.
Useful resources
Podcast: Advance Decision to Refuse Treatment with Celia Kitzinger
NHS: Advance Decision to Refuse Treatment
Compassion in Dying Living Will pack

Advance care plan tools/templates
- Some organisations have their own advance care plan template, so you could ask your healthcare professional if they could provide a copy for you.
- The following websites and resources may also be useful:
- Record your plans on this website: MyWishes: Free Will Writing, Digital Legacy, Advance Care Plan & Funeral Software
- Marie Curie: Marie Curie: planning your care in advance
- Hospice UK: Planning Ahead: What matters most to you | Welcome
- You can record your plans in this book: Funny end of life planner
Toolkits
-
Dementia Toolkit - 1510 Planning Ahead
-
Learning disability toolkit - Guide 3 (back to back printing at home booklet style)
-
Homeless Toolkit - Communicating about what matters to clients | Homeless Palliative Care Toolkit
-
Children and young people template which is used in South Yorkshire: CYPACP – Child & Young Persons Advance Care Plan
A lasting power of attorney (LPA) is a legal document that lets you (the ‘donor’) appoint one or more people (known as ‘attorneys’) to help you make decisions or to make decisions on your behalf.
This gives you more control over what happens to you if you have an accident or an illness and cannot make your own decisions (you ‘lack mental capacity’).
There are two types of LPA:
-
health and welfare
-
property and financial affairs
Why it matters
Your next of kin have no automatic right to speak for if you lose capacity through a sudden accident or a long-term disease, this can only be by consenting ahead through a Lasting Power of Attorney.
Without a LPA your next of kin will be unable to manage a joint bank account or pay essential bills
How to do it
There are three ways to make an LPA:
- Using the GOV.UK site
- Using an independent Lasting Power of Attorney Consultant
- Using a solicitor
When to consider it
- After the age of 18 and at any stage of life.
- Following diagnosis of a long-term health condition.
Organ Donation
Organ donation will be considered that you agree to become a potential organ donor when you die if:
- You are 18 or older
- You have not opted out
- You are not in an excluded group
Why it matters
Becoming an organ donor means you have the potential to save up to nine lives.
Anyone can register to become an organ donor, there is no age limit.
How to do it
Register your decision on the NHS Organ Donor Register.
Have the conversation with your family and friends, tell them what you have decided.
When to consider it
At any stage in life.
Resources
Reference – Organ donation text provided with permission by Clare Fuller, Advance Care Planning Explained | Plan with Confidence — Speak For Me LPA
Organ Donation Law in England
Podcast: Organ Donation: hope and transition after an unexpected death with Vicki Caldwell, mother of organ donor Fi
Mental Capacity
The Mental Capacity Act (MCA) is designed to protect and empower people who may lack the mental capacity to make their own decisions about their care and treatment. It applies to people aged 16 and over. It covers decisions about day-to-day things like what to wear or what to buy for the weekly shop, or serious life-changing decisions like whether to move into a care home or have major surgery.
The MCA says:
-
assume a person has the capacity to make a decision themselves, unless it's proved otherwise.
-
wherever possible, help people to make their own decisions.
-
do not treat a person as lacking the capacity to make a decision just because they make an unwise decision.
-
if you make a decision for someone who does not have capacity, it must be in their best interests.
-
treatment and care provided to someone who lacks capacity should be the least restrictive of their basic rights and freedoms.
Information provided with permission from www.nhs.uk
Resources
Text provided with permission by Clare Fuller and www.nhs.uk
Information about Lasting Power of Attorney
Make, register or end a Lasting Power of Attorney
Podcast: What can happen if you don’t have an LPA in place & a story of systematic failure
Blog: How much does it cost to make a Lasting Power of Attorney?
For more information go to Make, register or end a lasting power of attorney: Overview - GOV.UK
The NHS website explains that talking about death and dying can be difficult. Information provided by NHS is as follows -
Living with a terminal diagnosis and knowing you're dying can make you feel isolated, even though life is going on around you.
It can feel very difficult to speak about your illness or the fact you're dying, but talking with your loved ones can help. You or your family and friends may even find it a relief to have the subject out in the open, even if you find it upsetting.
Not talking can create worries or distance between you and the people who are important to you. Talking about your illness and death may help you feel more able to deal with the future and your worries together.
You might want to talk about a number of things. These might include:
-
feelings about death
-
worries
-
fears
-
your wishes for your future care
-
your funeral
-
things you would like to give to people
You do not have to talk about everything at once. Different situations work for different people, and there's no right or wrong way to start talking about dying.
If you find it hard to start the conversation, some of the following suggestions might help.
- Choose a time and a place when you will not be disturbed.
- Starting with a question may help because it gives the other person a chance to say how they feel. You could try saying something like:
-
"It would help me if we could talk about my situation. How do you feel about that?" or
-
"I know it might be difficult, but do you think we should talk about what's going to happen?"
-
Listen to what the other person says. If they change the subject or do not want to talk about it, try saying something like:
-
"OK, we do not have to talk about it now, but I hope we can talk about it another time. It's something I would really like to do."
-
It's normal for people to get upset or feel emotional when they talk about the death of someone they love. Try not to let this put you off.
Getting upset or crying can be a release from any worries or pressure people are feeling. Once this is out, it may help you feel able to discuss things more openly.
If you know you're coming to the end of your life, it's important to say the things you would like to the people you care about. This might be your partner, parents, brothers and sisters, children, grandchildren and friends.
You can tell people you love them. You might want to tell them they mean a lot to you or that a disagreement you had does not matter. It might feel very emotional.
If it becomes overwhelming, say so and suggest talking again another time. You could write a letter, make a video or fill a memory box with things that remind you of the times you've shared.
You can also think about dealing with any unfinished emotional business. If there's anyone you feel you need to apologise to, you can say you're sorry.
If you've had an argument with someone, you could consider getting back in touch. If the damage from an argument cannot be repaired, try not to worry about it. At least you know you've tried your best to make things right.
If you feel you're not ready to bring up the subject of your death with your loved ones, you might want to discuss it first with someone who is not as close to you, such as a chaplain, doctor, nurse or counsellor.
You can also talk to the Samaritans free of charge for emotional support by phone, email or in person.
Useful documents to help support conversations on death and dying
The charity Hospice UK runs a campaign called Dying Matters, which has information on talking about death and dying. There is information for carers, friends, those close to the person and family.
-
A booklet you may find useful to support these conversations can be found here: talking_about_death_booklet_final_version.pdf
-
If you are the person listening – these are some tips you may want to consider: The-importance-of-listening-3.jpg (800×2000)

Information to help you care for the person and to help you
Information to help you care for the person and to help you can be found at Support for carers | Hospice UK. The link includes information on:
-
how to care for someone at home,
-
juggling work and caring,
-
getting residential care,
-
when a person you are caring for dies,
-
looking after yourself when some is dying,
-
what to expect: death and dying.
Here is a helpful video on supporting someone to move, for yours and their safety and comfort: https://youtu.be/O13Ay35VtNE . Here are some tips on how to move someone safely:
-
Using the electric bed up and down as an aid to achieve safety and comfort,
-
Rolling the person too and thro for turning over for washing, changing,
-
Moving the person around the bed to make them more comfortable,
-
Helping a person to get in and out of bed and onto a wheelchair / chair / portable commode and back,
-
Helping out of a chair, to a portable commode,
-
Helping the person to move from the bed to the bathroom using a walking frame or wheelchair,
-
Showering.
Carers assessment and support
If you are caring for someone, then you are entitled to a carers assessment. The assessment will be a discussion about what your needs are as a carer and what help and support you may need to help you in your role.
To understand if you are a carer and to have an introduction to a carer assessments, take a look at the NHS website: https://www.nhs.uk/social-care-and-support/support-and-benefits-for-carers/carer-assessments/
The links to find out how to have a carer assessment in South Yorkshire are:
-
Barnsley https://www.barnsley.gov.uk/services/adult-social-care/information-for-carers/carers-assessment/
South Yorkshire information and support for carers
South Yorkshire information and support for carers can be found:
-
Barnsley Homepage - BarnsleyCarers
-
Doncaster Carers Offer
This information is taken from NHS England with permission
Coping financially with end of life care
Money can be a worry if you or a family member need to take time off work as a result of illness or to care for someone with a terminal illness. But there is support available.
Ask a GP, hospital doctor or nurse to refer you to a hospital social worker or community social worker.
They can assess your financial situation and give you advice on benefits. They can also tell you about any special funds you might qualify for.
You can also contact the social services department of your local council and ask for a care needs assessment. This will tell you if you’re eligible for any funding.
Benefits
You can check whether you're eligible for any of the benefits or payments listed below on the GOV.UK website:
-
Employment and Support Allowance (ESA) – if you're unable to work as a result of illness or disability
-
Statutory Sick Pay (SSP) – for some people who are employed
-
Personal Independence Payment (PIP) – help with extra living costs, you can get PIP more quickly if you have 12 months or less to live
-
Disability Living Allowance (DLA) for children – extra help for children under the age of 16 who need extra looking after or have walking difficulties
-
Carer's Allowance or Carer's Credit – if you're looking after someone
-
Attendance Allowance – for disabled people aged 65 or over, or who need care
-
Cost of Living Payments 2023 to 2024 – extra payments to help with the cost of living if you’re receiving certain benefits
Not everybody will be eligible for these benefits and, if you're eligible, claiming them might affect other benefits you receive. For example, getting a Carer's Allowance can affect the benefits of the person you're caring for.
You can use the Turn2us benefits calculator to see which benefits you might qualify for.
Special rules for end of life
If you’ve been told you have 12 months or less to live, you may be eligible for ‘special rules’.
This may mean your claim could be processed faster than usual or paid at a higher rate.
Financial Help from charities
Some charities can provide support for free, such as Marie Curie, Sue Ryder, Maggie's Centres, or your local hospice.
They can offer advice, counselling and practical help for people and their families who are living with illness.
Citizens Advice offers advice about financial help.
You may be able to apply for grants from charities, such as Turn2us grant search.
It’s a good idea to apply for any benefits you’re entitled to first before applying to charities for a grant.
Useful organisations
Enquiry phone lines
-
Pensions – 0800 731 7898
-
Macmillan support line - 0800 808 00 00
Fast track continuing health Care
In some medical situations you may be eligible for funding from the NHS to cover care costs. This is not in all situations and needs to be assessed by a medical professional and meet specific criteria.
If you have a rapidly deteriorating condition and the condition may be entering a terminal phase, then you may be eligible to receive urgent access to NHS continuing healthcare via fast-track.
An appropriate clinician will complete the fast-track pathway tool to establish your eligibility for NHS continuing healthcare. This clinician will send the completed fast-track pathway tool directly to your local Integrated Care Board (ICB), which should arrange for a care package to be provided for you, normally within 48 hours from receipt of the completed fast-track pathway tool.
Your ICB should review your care needs and the effectiveness of your care package. There may be some instances where it becomes appropriate to reassess your eligibility for NHS continuing healthcare using the decision support tool. If this is necessary, your ICB will carefully explain the process, as detailed in the ‘Assessments’ section above.
You can find out more about continuing healthcare fast-track on the GOV.UK website, here:
- NHS continuing healthcare fast-track pathway tool - GOV.UK
- Public information leaflet: NHS continuing healthcare and NHS-funded nursing care - GOV.UK
Information in this section is used with permission from: NHS continuing healthcare - Social care and support guide - NHS
Writing Wills
Finance and assets will - A will is a legal document which outlines where your assets (e.g. money, valuables) go after you have died. Having a will is for everyone, whatever amount of money / assets you have.
For those without a will, your assets (e.g. money, valuables) will be shared out according to certain rules (Who can inherit if there's no will - Citizens Advice). These rules may mean your assets are distributed not as you would have wished.
Take a look at these 10 reasons to write a will: 10 reasons to make a Will | Find out why you should make a Will | Remember A Charity
For more information on wills, including options on writing a will for free, please take a look at the following websites:
Digital will and social media legacy
Many people have social media profiles and online accounts. You may want to outline your wishes for what you want to happen to your social media and other online accounts after your death.
A simple template can be found here: Social Media Will - Digital Legacy Association or here: MyWishes - Social Media Will
Chaplains promote pastoral, spiritual and religious wellbeing through skilled compassionate person-centred care. This is available to patients, their families and carers, and to NHS staff, volunteers and students. They enable people to celebrate according to their religion or belief within NHS settings, and support those facing very difficult situations such as the death of a loved one, psychosis, being diagnosed with life-threatening conditions, and people who are receiving end of life care.
A short film (click here) was created with Chaplaincy teams and staff in the NHS South Yorkshire Integrated Care System, in partnership with Compassionate Sheffield, a local end-of-life multi-agency collaborative.
It explains the vital role the Chaplaincy service plays, setting out when it might be helpful to involve the chaplaincy team.
Below are links to the Chaplaincy services website within health services in South Yorkshire:
Barnsley
Doncaster
Rotherham
Sheffield
Religious and cultural approaches to death and bereavement
This tool provides helpful information on the death and dying religious practices of Buddhism, Christianity, Hinduism, Islam, Judaism, and Sikhism. You can view the tool here.
Verification and certification of the death - verification of death is when a medical professional confirms that the person has died. If the person has died in the community (in a home or care home) contact the medical professional whose contact details have been provided to you. This is usually a GP or district nurse (for expected deaths). If it is out of hours, phone 111.
A number of checks are completed. In South Yorkshire there will always be a medical professional attend.
For all deaths the following will also happen:
- Certification of death: this is where a medical examiner works with the GP / doctor to understand the cause of death and a death certificate is completed.
- The next of kin will also receive a phone call from the medical examiner’s offer where you can ask questions and raise concerns.
- The medical examiner process is completed for all deaths in England. The change happened in September 2024 where the process was introduced to all deaths in the community. Previously this was only used for hospital deaths. So, this may be a different process to what you may have experienced prior to this date.
- The death certificate will go direct to the local register office, where you can then arrange an appointment to register the death.
The GOV.UK website contains practical information on how to register a death: What to do after someone dies: Tell Us Once - GOV.UK
The AGE UK website has a dedicated page with helpful information of what to do when someone dies. You can view their website here.
The GOV.UK website also has information about the tell us once service. This is where you share details of the person who has died and, using a unique reference number, the details will be shared with a number of organisations including:
- HM Revenue and Customs (HMRC) - to deal with personal tax and to cancel benefits and credits, for example Child Benefit and tax credits
- Department for Work and Pensions (DWP) - to cancel benefits and entitlements, for example Universal Credit or State Pension
- Passport Office - to cancel a British passport
- Driver and Vehicle Licensing Agency (DVLA) - to cancel a licence, remove the person as the keeper of up to 5 vehicles and end the vehicle tax
- the local council - to cancel Housing Benefit, Council Tax Reduction (sometimes called Council Tax Support), a Blue Badge, inform council housing services and remove the person from the electoral register
- Veterans UK - to cancel or update Armed Forces Compensation Scheme payments
A suggested list of organisations you may need to contact directly may include:
- banks,
- building societies,
- mortgage companies,
- insurance,
- utility (gas, electric, TV, broadband provider, mobile phone provider)
How to arrange a funeral
- Ask the register office for details on how to arrange a funeral.
- An example of a planning check list can be found here: Funeral Planning Checklist | Central Co-op
- The Marie Curie website has some helpful information on how to arrange a funeral: How to arrange a funeral | Marie Curie
The links below are booklets which have been developed in South Yorkshire which will help you after the death of a person close to you:
Community Equipment returns
Families can return community equipment when someone has died so that it can be reused. Please contact your local service:
- Barnsley – South West Yorkshire Partnership NHS Foundation Trust: 01226 645400
- Doncaster – NRS Healthcare: TBC
- Rotherham – Medequip: 01709 916889
- Sheffield – Medequip: 0114 553 6449
Coping with loss
The death of someone close to us is one of the most stressful things we will ever experience. There is an increased risk of both mental and physical health problems following a bereavement.
Remember that grieving for someone can begin before they die, if you are aware that they are reaching the end of their life, if they have an incurable condition or are suffering from dementia.
What is grief?
The Cruse Bereavement Support website provides helpful information about understanding grief: Understanding grief - Cruse Bereavement Support
What does grief feel like?
You may find this video helpful to understand what grief feels like: What does grief feel like?
How do we share how we feel when we are grieving?
You may find this video helpful to help you communicate your grief: Communicating Grief
Tips to cope with loss and bereavement
The Cruse Bereavement Support website provides helpful information about managing your grief: Managing grief - Cruse Bereavement Support
Here are some tips to help you cope with loss and bereavement:
-
Give yourself time to go through the different stages of bereavement. They are a completely natural response and allowing yourself to feel and experience them will help in the grieving process.
-
You could try setting aside regular time with a photograph or object connected to the person who has died to think about them and acknowledge your feelings about them.
-
Some people are uncomfortable talking about death and grief. Try not to get frustrated if people don’t react the way you would like them to. Most people are doing their best to say and do the right thing.
-
Look after yourself – eat well, get out in nature, take time for yourself.
-
Remind yourself of the good things in life, whether that’s spending time with people who make you happy, eating your favourite food, visiting a special place.
-
Doing something to help other people can help. You could try volunteering at a food bank or homeless shelter or bake a cake for someone you care about.
-
Try going to a support group, online or in person. It can help to talk to people who have gone through a similar experience.
-
Be kind to yourself. Remember that this is one of the most distressing things you will go through in life and don’t expect too much of yourself
-
You may want to consider writing a journal and reflect on how our feelings have changed over time
-
You may find writing to the person who has died helps
-
You may want to explore different ways of remembering the person who has died. E.g. memory boxes, celebrating the first birthday, anniversary,
-
You may find talking to others about the person who has died helps. Talk to friends, relatives and those close to you, or in groups such as death cafes or community groups you may be involved in.
-
Seek professional support. You can find local support in the Local Bereavement Support section on this page.
How to help someone with their grief
Here are a couple of website suggestions with tips on how to support those who are grieving:
-
The NHS website has some helpful information and advice about grief after bereavement or loss, and information about national services who can offer support for anxiety, stress and depression: Get help with grief after bereavement or loss - NHS
Grief information in different languages
Cruse also provides a range of materials which can be read, downloaded and printed in different languages. Go to Help for those who don't speak English - Cruse Bereavement Support
Additional Resources
-
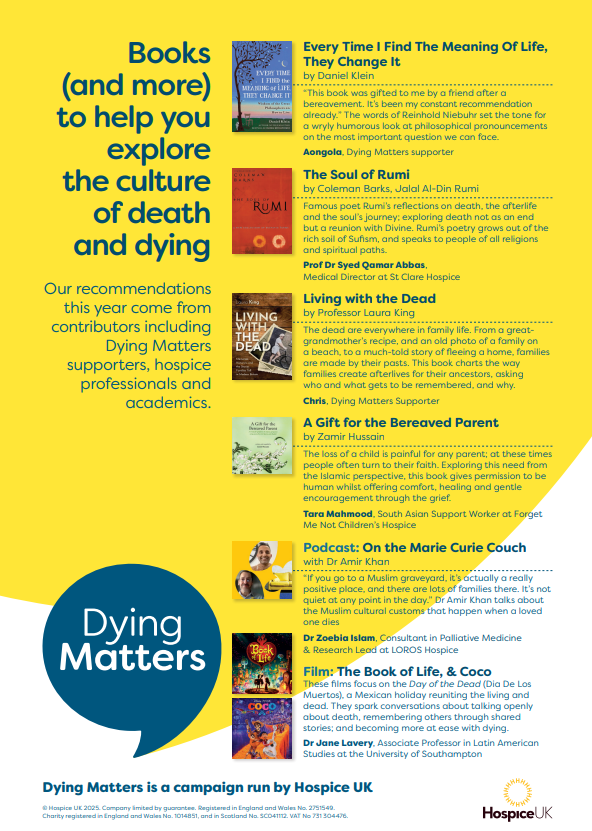
The Hospice UK website has a helpful recommended books guide to support people with bereavement and grief: Books and more poster - Dying Matters Awareness Week 2025 (low res).pdf
-
Health Unlocked: HealthUnlocked | The social network for health
How to talk to a child after a death
Apps
There are several apps and websites that can help young people
-
Apart of Me: Apart of Me | Helping young people cope with grief
-
Child Bereavement UK: Support for bereaved young people | Child Bereavement UK
Professional wellbeing
You can find national support via the following link:
Your Experience
Share your story about palliative care services in South Yorkshire through this online form: Tell us your stories :: South Yorkshire I.C.B
Experiences & learning of palliative and end of life care
You can read the report of experiences in Sheffield, by Healthwatch Sheffield, here.

What did we learn about?
The report contains information about a whole range of services people use at the end of life, as well as the wider support they and their families might have. This includes:
- Experiences of health services such as GPs, pharmacies, hospitals, and hospices.
- Experiences of social care and community organisations such as care homes, respite care, charities, and faith organisations.
- Advance care planning, for instance whether people were supported to choose where they wanted to die.
- Getting the right support, including what support was put in place, and the way support was delivered.
- Support for carers while supporting their friend or family member, as well as after they died.
- Ideas to improve palliative and end of life care.